Other
Incidence and Temporal Evolution of Delayed Peridevice Leak After Left Atrial Appendage Closure
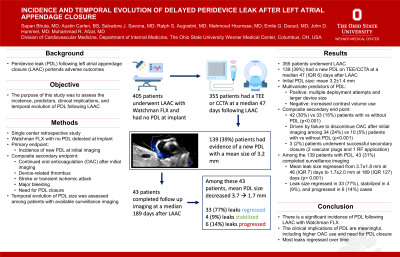
Purpose: Peridevice leak (PDL) following left atrial appendage closure (LAAC) portends adverse outcomes. The purpose of this study was to assess the incidence, predictors, clinical implications, and temporal evolution of PDL following LAAC.
Material and Methods: This single-center retrospective study included all patients who underwent LAAC with Watchman FLX and had no PDL detected at implant. The primary endpoint was incidence of new PDL at initial imaging. The composite secondary endpoint included continued oral anticoagulation (OAC) after initial imaging, device-related thrombus, stroke or transient ischemic attack, major bleeding, and need for PDL closure at longest follow-up. Temporal evolution of PDL was assessed in patients with available surveillance imaging.
Results: Among 355 patients who completed imaging at a median 47 (IQR 6) days after LAAC, 139 (39%) had a new PDL with a mean leak size of 3.2±1.4 mm [median 3.0 (IQR 2.0) mm, range 1.0-9.0 mm]. Multiple deployment attempts and larger device size were positive predictors of PDL, while increased contrast volume administration was a negative predictor of PDL. The composite secondary end point occurred in 42 (30%) and 33 (15%) patients with and without PDL respectively (p < 0.001). This was primarily driven by failure to discontinue OAC after initial imaging in patients with vs without PDL (with PDL: 34 (24%) vs without PDL: 10 (5%) patients, p< 0.001). Notably, 3 (2%) patients with PDL underwent successful secondary closure, 2 with a vascular plug and 1 with radiofrequency energy application to left atrial tissue adjacent to the leak, and 2 (1%) additional patients with PDL were referred for closure. Among the 139 patients with PDL, 43 (31%) completed surveillance imaging, and mean leak size regressed from 3.7±1.8mm at 46 (IQR 7) days to 1.7±2.0mm at 189 (IQR 127) days (p < 0.001). Notably, the leak size regressed in 33 (77%), remained stable in 4 (9%), and progressed in 6 (14%) cases.
Conclusions: There is a significant incidence of PDL following LAAC with Watchman FLX. The clinical implications of PDL are meaningful, including increased use of OAC after LAAC and need for PDL closure. Notably, regardless of initial size, most leaks regressed over time.
Material and Methods: This single-center retrospective study included all patients who underwent LAAC with Watchman FLX and had no PDL detected at implant. The primary endpoint was incidence of new PDL at initial imaging. The composite secondary endpoint included continued oral anticoagulation (OAC) after initial imaging, device-related thrombus, stroke or transient ischemic attack, major bleeding, and need for PDL closure at longest follow-up. Temporal evolution of PDL was assessed in patients with available surveillance imaging.
Results: Among 355 patients who completed imaging at a median 47 (IQR 6) days after LAAC, 139 (39%) had a new PDL with a mean leak size of 3.2±1.4 mm [median 3.0 (IQR 2.0) mm, range 1.0-9.0 mm]. Multiple deployment attempts and larger device size were positive predictors of PDL, while increased contrast volume administration was a negative predictor of PDL. The composite secondary end point occurred in 42 (30%) and 33 (15%) patients with and without PDL respectively (p < 0.001). This was primarily driven by failure to discontinue OAC after initial imaging in patients with vs without PDL (with PDL: 34 (24%) vs without PDL: 10 (5%) patients, p< 0.001). Notably, 3 (2%) patients with PDL underwent successful secondary closure, 2 with a vascular plug and 1 with radiofrequency energy application to left atrial tissue adjacent to the leak, and 2 (1%) additional patients with PDL were referred for closure. Among the 139 patients with PDL, 43 (31%) completed surveillance imaging, and mean leak size regressed from 3.7±1.8mm at 46 (IQR 7) days to 1.7±2.0mm at 189 (IQR 127) days (p < 0.001). Notably, the leak size regressed in 33 (77%), remained stable in 4 (9%), and progressed in 6 (14%) cases.
Conclusions: There is a significant incidence of PDL following LAAC with Watchman FLX. The clinical implications of PDL are meaningful, including increased use of OAC after LAAC and need for PDL closure. Notably, regardless of initial size, most leaks regressed over time.