Medical Management
Etripamil Use In Atrial Fibrillation With Rapid Ventricular Rate
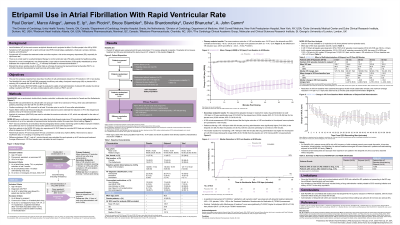
Marco Alings, MD, PhD, FESC – Professor, Department of Cardiology, Amphia Hospital, Breda, The Netherlands; James Ip, MD – Professor of Clinical Medicine, Division of Cardiology, Department of Medicine, Weill Cornell Medicine, New York Presbyterian Hospital, New York, USA; Jon Piccini, MD, MHS, FACC, FAHA, FHRS – Professor of Medicine, Duke University Medical Center and Duke Clinical Research Institute, Durham, NC; Bruce Stambler, MD – Doctor, Piedmont Heart Institute, Atlanta, GA, USA; Silvia Shardonofsky, MD, MSc – Medical Director, Milestone Pharmaceuticals, Montreal, Canada; David Bharucha, MD, PhD, FACC – Chief Medical Officer, Milestone Pharmaceuticals, Charlotte, NC, USA; A. John Camm, MD, FRCP – Professor of Clinical Cardiology, The Cardiology Clinical Academic Group, Molecular and Clinical Sciences Research Institute, St. George’s University of London, London, UK
Purpose: Atrial fibrillation (AF) is frequently associated with symptomatic episodes of rapid ventricular rate (RVR) despite currently available therapies. Etripamil nasal spray (NS) is a fast-acting, new chemical entity, nondihydropyridine calcium channel blocker under study in supraventricular tachycardia and AF-RVR.
Material and Methods: NODE-303 was a multi-center, multi-national, open-label study that allowed patients to self-administer a single 70 mg dose of etripamil to resolve up to 4 episodes of supraventricular tachycardia (SVT); 18 patients who self-treated for SVT were observed to have AF-RVR based on recorded ECG data. ReVeRA-201 was a randomized, double-blind, placebo-control multicenter study that was conducted in Canada and The Netherlands with a primary objective to demonstrate superiority of etripamil NS vs placebo in reducing VR in patients with AF-RVR; patients presenting to an ED with AF-RVR were screened and randomized 1:1 to receive double blinded etripamil 70 mg NS or placebo NS.
Results: In NODE-303, of 503 patients who treated at least one perceived episode of supraventricular tachycardia, 26 episodes of AF-RVR occurred in 18 patients, and 21 episodes had ECG data that could be interpreted. The mean age was 56.3 years and the mean baseline VR ± SEM was 129.7 ± 5.4 bpm. At 60 min following self-administration of etripamil NS, mean VR ± SEM was 110.2 ± 7.6 bpm (n=14). In ReVeRA-201, 87 patients were screened and 56 were randomized and dosed (27 with etripamil and 29 with placebo). In the efficacy population (N=49), the difference between the maximum mean reductions in ventricular rate (VR; baseline to nadir) over 60 min, etripamil vs placebo arms, adjusting for baseline VR, was -29.91 (95% CI: ‑40.31, -19.52; p< 0.0001). The higher VR reductions in etripamil vs placebo arms persisted for ≥150 min. Proportions of patients achieving a VR < 100 bpm during the first 60 min were 58.3% in the etripamil arm (median duration 45.5 min) vs 4.0% in the placebo arm (median duration 7 min in 1 patient) (p < 0.0001). Serious AEs were rare (1 patient, etripamil arm; 2 patients placebo arm).
Conclusions: In both studies, etripamil NS significantly reduced VR rapidly after drug administration, which is consistent with its pharmacologic profile.
Material and Methods: NODE-303 was a multi-center, multi-national, open-label study that allowed patients to self-administer a single 70 mg dose of etripamil to resolve up to 4 episodes of supraventricular tachycardia (SVT); 18 patients who self-treated for SVT were observed to have AF-RVR based on recorded ECG data. ReVeRA-201 was a randomized, double-blind, placebo-control multicenter study that was conducted in Canada and The Netherlands with a primary objective to demonstrate superiority of etripamil NS vs placebo in reducing VR in patients with AF-RVR; patients presenting to an ED with AF-RVR were screened and randomized 1:1 to receive double blinded etripamil 70 mg NS or placebo NS.
Results: In NODE-303, of 503 patients who treated at least one perceived episode of supraventricular tachycardia, 26 episodes of AF-RVR occurred in 18 patients, and 21 episodes had ECG data that could be interpreted. The mean age was 56.3 years and the mean baseline VR ± SEM was 129.7 ± 5.4 bpm. At 60 min following self-administration of etripamil NS, mean VR ± SEM was 110.2 ± 7.6 bpm (n=14). In ReVeRA-201, 87 patients were screened and 56 were randomized and dosed (27 with etripamil and 29 with placebo). In the efficacy population (N=49), the difference between the maximum mean reductions in ventricular rate (VR; baseline to nadir) over 60 min, etripamil vs placebo arms, adjusting for baseline VR, was -29.91 (95% CI: ‑40.31, -19.52; p< 0.0001). The higher VR reductions in etripamil vs placebo arms persisted for ≥150 min. Proportions of patients achieving a VR < 100 bpm during the first 60 min were 58.3% in the etripamil arm (median duration 45.5 min) vs 4.0% in the placebo arm (median duration 7 min in 1 patient) (p < 0.0001). Serious AEs were rare (1 patient, etripamil arm; 2 patients placebo arm).
Conclusions: In both studies, etripamil NS significantly reduced VR rapidly after drug administration, which is consistent with its pharmacologic profile.