Other
Cost Analysis of Left Atrial Ablation Procedures Using Proactive Esophageal Cooling
Daniel Moehringer, Student – Student, Virginia Tech; Julie Cooper, MD – Physician, University of Texas Southwestern Medical Center; Danya Willms, RCES – Nurse, Sharp Memorial Hospital; Jason Zagrodzky, MD – Electrophysiologist, Texas Cardiac Arrhythmia; Christopher Joseph, MD – Physician, University of Texas Southwestern Medical Center; Rishi Sikka, MD – Physician, Brown University; Annie Ruppert, RN – Nurse, Sharp Memorial Hospital; Erik Kulstad, MD, MS – Physician, University of Texas Southwestern Medical Center; Gregory Francisco, MD – Electrophysiologist, Sharp Memorial Hospital; Charles Athill, MD – Electrophysiologist, Sharp Memorial Hospital; Shane Bailey, MD – Electrophysiologist, Texas Cardiac Arrhythmia; Jacob Sherman, Student – Student, Washington University in St. Louis; Alex Ro, MD – Electrophysiologist, NorthShore University Hospital; Westby Fisher, MD – Electrophysiologist, NorthShore University Hospital; Jose Nazari, MD – Electrophysiologist, NorthShore University Hospital; James Daniels, MD – Electrophysiologist, University of Texas Southwestern Medical Center; Robert Turer, MD – Electrophysiologist, University of Texas Southwestern Medical Center; Samuel McDonald, MD – Electrophysiologist, University of Texas Southwestern Medical Center; Raymond Kawasaki, MD – Electrophysiologist, NorthShore University Hospital; Christopher Henry, MD – Electrophysiologist, Northwest Community Hospital; Mark Metzl, MD – Electrophysiologist, NorthShore University Hospital
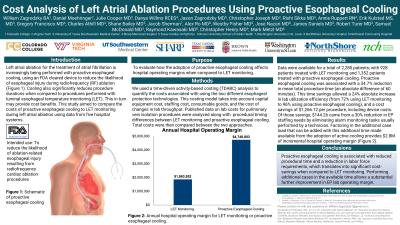
Purpose: Left atrial ablation for the treatment of atrial fibrillation is increasingly being performed with proactive esophageal cooling, which is FDA cleared to reduce the likelihood of esophageal injury during radiofrequency (RF) ablation. Cooling also significantly reduces procedure duration when compared to procedures performed with luminal esophageal temperature monitoring (LET). This in turn may provide cost benefits. This study aimed to compare the costs of proactive esophageal cooling to LET monitoring during left atrial ablation using data from five hospital systems.
Material and Methods: We used a time-driven activity-based costing (TDABC) analysis to quantify the costs associated with using the two different esophageal protection technologies. This costing model takes into account capital equipment cost, staffing cost, consumable goods, and the cost of changes in lab throughput. Published data on lab costs for pulmonary vein isolation procedures were analyzed along with procedural timing differences between LET monitoring and proactive esophageal cooling. Total costs were then compared between the two approaches.
Results: Data were available for a total of 2,280 patients; with 928 patients treated with LET monitoring and 1,352 patients treated with proactive esophageal cooling. Proactive esophageal cooling was associated with a 34.7% reduction in mean total procedure time (an absolute difference of 60 minutes). This time savings allowed a 24% absolute increase in lab utilization efficiency (from 72% using LET monitoring to 96% using proactive esophageal cooling), and a cost savings of $1,266.12 per procedure, including device costs. Of those savings, $144.26 came from a 30% reduction in EP staffing needs by eliminating alarm monitoring tasks usually performed by a technician. Factoring in the additional case load that can be added with this additional time made available from the adoption of active cooling provides $2.8M of incremental hospital operating margin.
Conclusions: Proactive esophageal cooling is associated with reduced procedural time and a reduction in labor force requirements, which translates into significant cost-savings when compared to LET monitoring. Performing additional cases in the available time allows a substantial further improvement in EP lab operating margin.
Material and Methods: We used a time-driven activity-based costing (TDABC) analysis to quantify the costs associated with using the two different esophageal protection technologies. This costing model takes into account capital equipment cost, staffing cost, consumable goods, and the cost of changes in lab throughput. Published data on lab costs for pulmonary vein isolation procedures were analyzed along with procedural timing differences between LET monitoring and proactive esophageal cooling. Total costs were then compared between the two approaches.
Results: Data were available for a total of 2,280 patients; with 928 patients treated with LET monitoring and 1,352 patients treated with proactive esophageal cooling. Proactive esophageal cooling was associated with a 34.7% reduction in mean total procedure time (an absolute difference of 60 minutes). This time savings allowed a 24% absolute increase in lab utilization efficiency (from 72% using LET monitoring to 96% using proactive esophageal cooling), and a cost savings of $1,266.12 per procedure, including device costs. Of those savings, $144.26 came from a 30% reduction in EP staffing needs by eliminating alarm monitoring tasks usually performed by a technician. Factoring in the additional case load that can be added with this additional time made available from the adoption of active cooling provides $2.8M of incremental hospital operating margin.
Conclusions: Proactive esophageal cooling is associated with reduced procedural time and a reduction in labor force requirements, which translates into significant cost-savings when compared to LET monitoring. Performing additional cases in the available time allows a substantial further improvement in EP lab operating margin.