Medical Management
Concomitant Antiarrhythmic Use Among Patients Who Received Etripamil For Atrial Fibrillation With Rapid Ventricular Rate
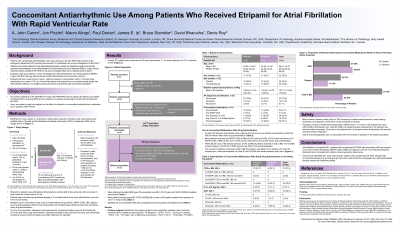
Jon Piccini, MD, MHS, FACC, FAHA, FHRS – Professor of Medicine, Duke University Medical Center and Duke Clinical Research Institute, Durham, NC; Marco Alings, MD, PhD, FESC – Professor, Doctor, Department of Cardiology, Amphia Hospital, Breda, The Netherlands; Paul Dorian, MD, MSc, FRCP(C) – Professor, The Division of Cardiology, Unity Health Toronto, Toronto, Canada; James Ip, MD – Professor of Clinical Medicine, Division of Cardiology, Department of Medicine, Weill Cornell Medicine, New York Presbyterian Hospital, New York, USA; Bruce Stambler, MD – Doctor, Piedmont Heart Institute, Atlanta, GA, USA; David Bharucha, MD, PhD, FACC – Chief Medical Officer, Milestone Pharmaceuticals, Charlotte, NC, USA; Denis Roy, MD, FRCPC, FHRS – Professor of Medicine, Department of Medicine, Montreal Heart Institute, Montreal, Québec, Canada
Purpose: Patients with atrial fibrillation (AF) often experience recurrent episodes of symptomatic rapid ventricular rate (RVR) despite treatment. Etripamil nasal spray (NS) is a rapid-acting, nondihydropyridine (NDHP) calcium channel blocker (CCB) formulated for self-administration that is currently under study for treatment of paroxysmal supraventricular tachycardia and AF-RVR.
Material and Methods: ReVeRA-201 was a randomized, double-blind, placebo-controlled multicenter study assessing the superiority of etripamil NS vs placebo in reducing ventricular rate in patients with AF-RVR. Patients who presented to an emergency department with AF and ventricular rate ≥110 bpm were screened and randomized 1:1 to receive double blinded etripamil 70 mg NS or placebo NS. In this analysis, the use of concomitant antiarrhythmic drugs (AADs), including NDHP CCBs, beta blockers (BBs), digoxin, and oral anticoagulants (OACs), during the 24 hours following study drug administration was compared between patients who received etripamil NS or placebo.
Results: Patients (n=56) with symptomatic AF-RVR were randomized to receive etripamil (N=27) or placebo (N=29). Patients had a mean (SD) age of 64.6 (10.5) years, and 60.7% were men. Study groups were comparable at baseline, with most patients being diagnosed with paroxysmal AF (75.0%, n=42) or persistent AF (17.9%, n=10), and having a mean (SD) systolic blood pressure of 127.71 (18.52). At enrollment, use of AADs was similar between groups at baseline, with patients in the placebo group receiving OACs (55.1%, n=16), any NDHP CCB or BB (44.8%, n=13), and any Class IC or III AAD (17.2%; n=5); and patients in the etripamil group receiving OACs (59.3%, n=16), any NDHP CCB or BB (55.6%, n=15), and any Class IC or III AAD (29.6%, n=8). Per protocol, no patients were administered additional medications within 60 minutes. Following 1 hour, up to 24 hours of study drug administration, fewer patients in the etripamil group received any NDHP CCB or BB (22.2%, n=6) or digoxin (11.1%, n=3) than patients in the placebo group NDHP CCB or BB (51.7%, n=15) or digoxin, (20.7%, n=6). Use of AADs was similar between groups (placebo, 27.6%, n=8; etripamil, 29.6%, n=8).
Conclusions: Patients with symptomatic AF-RVR who received etripamil NS had less frequent use of NDHP CCBs, BB, and digoxin in the 24 hours following treatment than patients who received placebo.
Material and Methods: ReVeRA-201 was a randomized, double-blind, placebo-controlled multicenter study assessing the superiority of etripamil NS vs placebo in reducing ventricular rate in patients with AF-RVR. Patients who presented to an emergency department with AF and ventricular rate ≥110 bpm were screened and randomized 1:1 to receive double blinded etripamil 70 mg NS or placebo NS. In this analysis, the use of concomitant antiarrhythmic drugs (AADs), including NDHP CCBs, beta blockers (BBs), digoxin, and oral anticoagulants (OACs), during the 24 hours following study drug administration was compared between patients who received etripamil NS or placebo.
Results: Patients (n=56) with symptomatic AF-RVR were randomized to receive etripamil (N=27) or placebo (N=29). Patients had a mean (SD) age of 64.6 (10.5) years, and 60.7% were men. Study groups were comparable at baseline, with most patients being diagnosed with paroxysmal AF (75.0%, n=42) or persistent AF (17.9%, n=10), and having a mean (SD) systolic blood pressure of 127.71 (18.52). At enrollment, use of AADs was similar between groups at baseline, with patients in the placebo group receiving OACs (55.1%, n=16), any NDHP CCB or BB (44.8%, n=13), and any Class IC or III AAD (17.2%; n=5); and patients in the etripamil group receiving OACs (59.3%, n=16), any NDHP CCB or BB (55.6%, n=15), and any Class IC or III AAD (29.6%, n=8). Per protocol, no patients were administered additional medications within 60 minutes. Following 1 hour, up to 24 hours of study drug administration, fewer patients in the etripamil group received any NDHP CCB or BB (22.2%, n=6) or digoxin (11.1%, n=3) than patients in the placebo group NDHP CCB or BB (51.7%, n=15) or digoxin, (20.7%, n=6). Use of AADs was similar between groups (placebo, 27.6%, n=8; etripamil, 29.6%, n=8).
Conclusions: Patients with symptomatic AF-RVR who received etripamil NS had less frequent use of NDHP CCBs, BB, and digoxin in the 24 hours following treatment than patients who received placebo.