Cardiac: Other
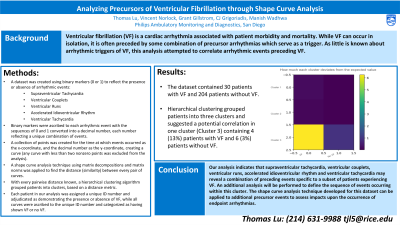
Analyzing Precursors of Ventricular Fibrillation through Shape Curve Analysis
Vincent Norlock, BS Eng – Strategic Business Development Lead, Philips; Grant Gillstrom, MS – Business Intelligence Lead, Philips; CJ Grigoriadis, MSc, CRAT – Clinical Solutions Manager, Philips; Manish Wadhwa, MD, FHRS, FACC – Head of Medical & Clinical AM&D, Philips
Purpose: Ventricular fibrillation (VF) is a cardiac arrhythmia associated with patient morbidity and mortality. While VF can occur in isolation, it is often preceded by some combination of precursor arrhythmias which serve as a trigger. As little is known about arrhythmic triggers of VF, this analysis attempted to correlate arrhythmic events preceding VF.
Material and Methods: A dataset was created using binary markers (0 or 1) to reflect the presence or absence of arrhythmic events. Binary markers were ascribed to arrhythmic events (supraventricular tachycardia, ventricular couplets, ventricular runs, accelerated idioventricular rhythm, ventricular tachycardia), with the sequences of 0 and 1 converted into a decimal number, each number reflecting a unique combination of events. A corresponding shape curve analysis technique was used to analyze the series of events. A collection of points was created for the time at which events occurred as the x-coordinate, and the decimal number as the y-coordinate. Curves were generated by connecting points with straight lines. Any curve with less than two nonzero points was excluded from the analysis. A shape curve analysis technique using matrix decompositions and matrix norms was applied to find the distance between two curves. With every pairwise distance known, a hierarchical clustering algorithm grouped patients into clusters, based on a distance metric. Each patient in our analysis was assigned a unique ID number and adjudicated as demonstrating the presence or absence of VF, while all curves were ascribed to the unique ID number and categorized as having shown VF or no VF. VF was defined as a disorganized and chaotic rhythm with no P waves or QRS complexes present.
Results: The dataset contained 30 patients with VF and 204 patients without VF. Hierarchical clustering grouped patients into three clusters and suggested a potential correlation in one cluster containing 4 (13%) patients with VF and 6 (3%) without.
Conclusions: Our analysis indicates that supraventricular tachycardia, ventricular couplets, ventricular runs, accelerated idioventricular rhythm and ventricular tachycardia may reveal a combination of preceding events specific to a subset of patients experiencing VF. The shape curve analysis technique developed for this dataset can be applied to additional precursor events to assess impacts upon the occurrence of endpoint arrhythmias.
Material and Methods: A dataset was created using binary markers (0 or 1) to reflect the presence or absence of arrhythmic events. Binary markers were ascribed to arrhythmic events (supraventricular tachycardia, ventricular couplets, ventricular runs, accelerated idioventricular rhythm, ventricular tachycardia), with the sequences of 0 and 1 converted into a decimal number, each number reflecting a unique combination of events. A corresponding shape curve analysis technique was used to analyze the series of events. A collection of points was created for the time at which events occurred as the x-coordinate, and the decimal number as the y-coordinate. Curves were generated by connecting points with straight lines. Any curve with less than two nonzero points was excluded from the analysis. A shape curve analysis technique using matrix decompositions and matrix norms was applied to find the distance between two curves. With every pairwise distance known, a hierarchical clustering algorithm grouped patients into clusters, based on a distance metric. Each patient in our analysis was assigned a unique ID number and adjudicated as demonstrating the presence or absence of VF, while all curves were ascribed to the unique ID number and categorized as having shown VF or no VF. VF was defined as a disorganized and chaotic rhythm with no P waves or QRS complexes present.
Results: The dataset contained 30 patients with VF and 204 patients without VF. Hierarchical clustering grouped patients into three clusters and suggested a potential correlation in one cluster containing 4 (13%) patients with VF and 6 (3%) without.
Conclusions: Our analysis indicates that supraventricular tachycardia, ventricular couplets, ventricular runs, accelerated idioventricular rhythm and ventricular tachycardia may reveal a combination of preceding events specific to a subset of patients experiencing VF. The shape curve analysis technique developed for this dataset can be applied to additional precursor events to assess impacts upon the occurrence of endpoint arrhythmias.